Foot injuries from rock climbing are more common than many people think, especially during falls or from wearing tight climbing shoes. Falls can lead to bruises, sprains, or broken bones in the heel or ankle, which may require surgery to heal properly. However, repeated impact and pressure from tight shoes can also cause long-term problems. These include pain in the toes, thickened skin, and blood under the toenails. Many climbers wear shoes that are too small in order to get a better grip, but this can change how the foot moves and put too much pressure on certain areas. Over time, this can lead to chronic foot pain and deformities that may limit movement or cause discomfort even when not climbing. Changes in toe shape, such as bunions, or stiffness in the big toe joint may also develop. A podiatrist can diagnose climbing-related foot and ankle injuries, help manage pain, and recommend the best medical treatment, which may include surgery if needed. If you have injured your foot while rock climbing, whether indoors or outside, it is suggested that you make an appointment with a podiatrist for treatment.
Foot Pain
Foot pain can be extremely painful and debilitating. If you have a foot pain, consult with Massimo Pietrantoni, DPM from Rochester Podiatry, LLP. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
Causes
Foot pain is a very broad condition that could be caused by one or more ailments. The most common include:
Diagnosis
To figure out the cause of foot pain, podiatrists utilize several different methods. This can range from simple visual inspections and sensation tests to X-rays and MRI scans. Prior medical history, family medical history, and any recent physical traumatic events will all be taken into consideration for a proper diagnosis.
Treatment
Treatment depends upon the cause of the foot pain. Whether it is resting, staying off the foot, or having surgery; podiatrists have a number of treatment options available for foot pain.
If you have any questions, please feel free to contact one of our offices located in Brighton and Greece of Rochester, NY . We offer the newest diagnostic and treatment technologies for all your foot care needs.
The feet, being the foundation of the body, carry all of the body’s weight and are therefore prone to experiencing pain and discomfort. If you are experiencing foot pain, it is important to determine where in the foot you are experiencing this pain to help discover the cause of it. While pain can be experienced virtually anywhere in the foot, the most common sites of foot pain are in the heel and ankle.
Heel pain can be due to a multitude of conditions including plantar fasciitis, Achilles tendinitis, and heel spurs. Pain experienced in the ankle can be a sign of an ankle sprain, arthritis, gout, ankle instability, ankle fracture, or nerve compression. In more serious cases, pain in the foot can be a sign of improper alignment or an infection.
Foot pain can be accompanied by symptoms including redness, swelling, stiffness and warmth in the affected area. Whether the pain can be described as sharp or dull depends on the foot condition behind it. It is important to visit your local podiatrist if your foot pain and its accompanying symptoms persist and do not improve over time.
Depending on the location and condition of your foot pain, your podiatrist may prescribe certain treatments. These treatments can include but are not limited to prescription or over-the-counter drugs and medications, certain therapies, cortisone injections, or surgery.
If you are experiencing persistent foot pain, it is important to consult with your foot and ankle doctor to determine the cause and location. He or she will then prescribe the best treatment for you. While milder cases of foot pain may respond well to rest and at-home treatments, more serious cases may take some time to fully recover.

Bunions are bony bumps that form at the base of the big toe, as the tip of the toe angles toward the second toe. Over time, bunions can become more noticeable, and the skin over the bump may appear red and inflamed. The area can be painful, especially when pressure is applied, making it difficult to wear certain shoes or walk comfortably. Bunions are common in individuals who wear tight or ill-fitting shoes, particularly women who wear high heels. However, they can also be caused by genetic factors, abnormal foot structure, or conditions like arthritis. The symptoms include pain, swelling, and the appearance of a hard bump at the joint of the big toe. A podiatrist can help by diagnosing the condition and offering treatments such as custom orthotics, padding, or even surgery in severe cases. If you are dealing with this condition, it is suggested that you make an appointment with a podiatrist.
If you are suffering from bunion pain, contact Massimo Pietrantoni, DPM of Rochester Podiatry, LLP. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is a Bunion?
Bunions are painful bony bumps that usually develop on the inside of the foot at the joint of the big toe. As the deformity increases over time, it may become painful to walk and wear shoes. Women are more likely to exacerbate existing bunions since they often wear tight, narrow shoes that shift their toes together. Bunion pain can be relieved by wearing wider shoes with enough room for the toes.
Causes
Symptoms
In order to diagnose your bunion, your podiatrist may ask about your medical history, symptoms, and general health. Your doctor might also order an x-ray to take a closer look at your feet. Nonsurgical treatment options include orthotics, padding, icing, changes in footwear, and medication. If nonsurgical treatments don’t alleviate your bunion pain, surgery may be necessary.
If you have any questions, please feel free to contact one of our offices located in Brighton and Greece of Rochester, NY . We offer the newest diagnostic and treatment technologies for all your foot care needs.
A bunion is an enlargement of the base joint of the toe that connects to the foot, often formed from a bony growth or a patch of swollen tissues. It is caused by the inward shifting of the bones in the big toe, toward the other toes of the foot. This shift can cause a serious amount of pain and discomfort. The area around the big toe can become inflamed, red, and painful.
Bunions are most commonly formed in people who are already genetically predisposed to them or other kinds of bone displacements. Existing bunions can be worsened by wearing improperly fitting shoes. Trying to cram your feet into high heels or running or walking in a way that causes too much stress on the feet can exacerbate bunion development. High heels not only push the big toe inward, but shift one's body weight and center of gravity towards the edge of the feet and toes, expediting bone displacement.
A podiatrist knowledgeable in foot structure and biomechanics will be able to quickly diagnose bunions. Bunions must be distinguished from gout or arthritic conditions, so blood tests may be necessary. The podiatrist may order a radiological exam to provide an image of the bone structure. If the x-ray demonstrates an enlargement of the joint near the base of the toe and a shifting toward the smaller toes, this is indicative of a bunion.
Wearing wider shoes can reduce pressure on the bunion and minimize pain, and high heeled shoes should be eliminated for a period of time. This may be enough to eliminate the pain associated with bunions; however, if pain persists, anti-inflammatory drugs may be prescribed. Severe pain may require an injection of steroids near the bunion. Orthotics for shoes may be prescribed which, by altering the pressure on the foot, can be helpful in reducing pain. These do not correct the problem; but by eliminating the pain, they can provide relief.
For cases that do not respond to these methods of treatment, surgery can be done to reposition the toe. A surgeon may do this by taking out a section of bone or by rearranging the ligaments and tendons in the toe to help keep it properly aligned. It may be necessary even after surgery to wear more comfortable shoes that avoid placing pressure on the toe, as the big toe may move back to its former orientation toward the smaller toes.
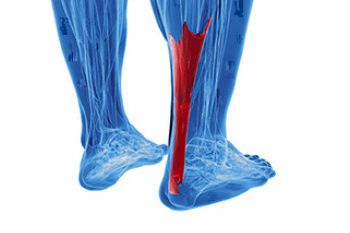
An Achilles tendon tear is a painful injury that often occurs during activities that involve sudden starts, stops, or pivots, especially in sports or while running. The Achilles tendon, which connects the calf muscles to the heel bone, is essential for walking, running, and rising onto the toes. A torn Achilles tendon may happen suddenly, often with a popping sound, followed by sharp pain at the back of the ankle. Patients may find it difficult to push off the foot or stand on their toes. In many cases, the foot may exhibit abnormal movement, including excessive pronation or supination, which can place strain on the tendon. A podiatrist can examine your ankle and foot alignment, assess range of motion, and determine the extent of the tear using diagnostic tests. If the tendon is completely torn, surgery may be required to restore function. A podiatrist can also help guide you through non-surgical recovery methods, including immobilization, and provide support for proper foot biomechanics. If you have injured your Achilles tendon, it is suggested that you make an immediate appointment with a podiatrist for an exam, diagnosis, and treatment.
Achilles tendon injuries need immediate attention to avoid future complications. If you have any concerns, contact Massimo Pietrantoni, DPM of Rochester Podiatry, LLP. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is the Achilles Tendon?
The Achilles tendon is a tendon that connects the lower leg muscles and calf to the heel of the foot. It is the strongest tendon in the human body and is essential for making movement possible. Because this tendon is such an integral part of the body, any injuries to it can create immense difficulties and should immediately be presented to a doctor.
What Are the Symptoms of an Achilles Tendon Injury?
There are various types of injuries that can affect the Achilles tendon. The two most common injuries are Achilles tendinitis and ruptures of the tendon.
Achilles Tendinitis Symptoms
Rupture Symptoms
Treatment and Prevention
Achilles tendon injuries are diagnosed by a thorough physical evaluation, which can include an MRI. Treatment involves rest, physical therapy, and in some cases, surgery. However, various preventative measures can be taken to avoid these injuries, such as:
If you have any questions please feel free to contact one of our offices located in Brighton and Greece of Rochester, NY . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
The Achilles tendon is the largest tendon in the body; it is a tough band of fibrous tissue that stretches from the bones of the heel to the calf muscles. This tendon is what allows us to stand on our toes while running, walking, or jumping, it is common for this tendon to become injured. In severe cases, the Achilles tendon may become partially torn or completely ruptured. However, this tendon is susceptible to injury because of its limited blood supply and the high level of tension it endures.
The people who are more likely to suffer from Achilles tendon injuries are athletes who partake in activities that require them to speed up, slow down, or pivot. Consequently, athletes who engage in running, gymnastics, dance, football, baseball, basketball, or tennis are more likely to suffer from Achilles tendon injuries. Additionally, there are other factors that may make you more prone to this injury. People who wear high heels, have flat feet, tight leg muscles or tendons, or take medicines called glucocorticoids are more likely to have Achilles tendon injuries.
A common symptom of an Achilles tendon injury is pain above the heel that is felt when you stand on your toes. However, if the tendon is ruptured, the pain will be severe, and the area may become swollen and stiff. Other symptoms may be reduced strength in the lower ankle or leg area, and reduced range of motion in the ankle. When the Achilles tendon tears, there is usually a popping sound that occurs along with it. People who have acute tears or ruptures may find walking and standing to be difficult.
If you suspect you have injured your Achilles tendon, you should see your podiatrist to have a physical examination. Your podiatrist will likely conduct a series of tests to diagnose your injury including a “calf-squeeze” test. Calf squeeze tests are performed by first squeezing the calf muscle on the healthy leg. This will pull on the tendon and consequently cause the foot to move. Afterward, the same test will be performed on the injured leg. If the tendon is torn, the foot won’t move because the calf muscle won’t be connected to the foot.

Falling can cause significant injury to the feet, leading to sprains, fractures, and long-term discomfort. The impact of a fall may result in ligament damage, bone fractures, or joint misalignment, affecting mobility and overall foot function. Several risk factors increase the likelihood of falling, including poor balance, muscle weakness, and certain medical conditions that affect coordination. Hazards within the home, such as loose rugs, poor lighting, and cluttered pathways, further contribute to the risk. Prevention methods include keeping walkways clear, wearing proper footwear with supportive soles, and improving strength and balance through regular exercise. Installing handrails and ensuring adequate lighting can also reduce the chances of falling. If you have hurt your feet from falling, it is suggested that you consult a podiatrist who can treat various foot conditions, and guide you toward effective fall prevention methods.
Preventing falls among the elderly is very important. If you are older and have fallen or fear that you are prone to falling, consult with Massimo Pietrantoni, DPM from Rochester Podiatry, LLP. Our doctor will assess your condition and provide you with quality advice and care.
Every 11 seconds, an elderly American is being treated in an emergency room for a fall related injury. Falls are the leading cause of head and hip injuries for those 65 and older. Due to decreases in strength, balance, senses, and lack of awareness, elderly persons are very susceptible to falling. Thankfully, there are a number of things older persons can do to prevent falls.
How to Prevent Falls
Some effective methods that older persons can do to prevent falls include:
Falling can be a traumatic and embarrassing experience for elderly persons; this can make them less willing to leave the house, and less willing to talk to someone about their fears of falling. Doing such things, however, will increase the likelihood of tripping or losing one’s balance. Knowing the causes of falling and how to prevent them is the best way to mitigate the risk of serious injury.
If you have any questions, please feel free to contact one of our offices located in Brighton and Greece of Rochester, NY . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Elderly Americans are very susceptible to falls as they get older. Everyone experiences decreases in flexibility, balance, strength, and the senses as they age. This correlates to some eye-opening statistics. 1 in 4 Americans aged 65 and older fall each year. An elderly American is being treated for a fall in an emergency room every 11 seconds. In light of these striking statistics, one can see the importance of taking steps to prevent falls.
Finding an exercise program for the elderly is an excellent way to reduce the likelihood of falls. Look for an exercise program that improves strength and balance. Elderly people who live a more sedentary lifestyle, with little physical activity, are at an increased risk of falling. Wearing well-fitted footwear that provides good foot support and cushion will help prevent falls from poorly fitted shoes. Talking to a podiatrist about your susceptibility to falls and about inspecting your prescriptions will help to avoid any medication that could make falls more likely. Due to a decline in the senses among the elderly, having your eyes and hearing checked is recommended.
Around half of all falls occur in the household. Removing tripping hazards in the home and making it more accommodating to older persons can significantly reduce falls. Some notable household changes include increasing lighting around the house, installing grab bars in the shower and bathroom, and making sure the floor is clear of clutter. Other smart options include installing a shower chair, using rubber-bottomed rugs, and placing railings on both sides of stairwells.
Finally, discuss with a doctor and your family about your fear of falling. This will help to increase awareness among the population on the need for fall prevention. A lack of awareness on the matter, and a downplaying of importance are what increase the risks of falling. Following these tips can help to reduce the risk for yourself and your loved ones.

Charcot foot is a serious condition that affects people with peripheral neuropathy, most commonly those with diabetes. It weakens the bones in the foot, causing them to fracture and dislocate without significant pain. As the condition progresses, the arch collapses, leading to a rocker-bottom type of deformity. Early signs include swelling, redness, and warmth in the foot, often mistaken for infection. If left untreated, Charcot foot can lead to severe deformity, ulceration, and an increased risk of limb loss. Early diagnosis and treatment are critical. Offloading the foot with a total contact cast or custom orthotic device helps protect and stabilize the bones during healing. In advanced cases, surgery may be necessary. If you have diabetes and notice changes in your feet, it is suggested that you see a podiatrist for a proper diagnosis and treatment.
Wound care is an important part in dealing with diabetes. If you have diabetes and a foot wound or would like more information about wound care for diabetics, consult with Massimo Pietrantoni, DPM from Rochester Podiatry, LLP. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
What Is Wound Care?
Wound care is the practice of taking proper care of a wound. This can range from the smallest to the largest of wounds. While everyone can benefit from proper wound care, it is much more important for diabetics. Diabetics often suffer from poor blood circulation which causes wounds to heal much slower than they would in a non-diabetic.
What Is the Importance of Wound Care?
While it may not seem apparent with small ulcers on the foot, for diabetics, any size ulcer can become infected. Diabetics often also suffer from neuropathy, or nerve loss. This means they might not even feel when they have an ulcer on their foot. If the wound becomes severely infected, amputation may be necessary. Therefore, it is of the upmost importance to properly care for any and all foot wounds.
How to Care for Wounds
The best way to care for foot wounds is to prevent them. For diabetics, this means daily inspections of the feet for any signs of abnormalities or ulcers. It is also recommended to see a podiatrist several times a year for a foot inspection. If you do have an ulcer, run the wound under water to clear dirt from the wound; then apply antibiotic ointment to the wound and cover with a bandage. Bandages should be changed daily and keeping pressure off the wound is smart. It is advised to see a podiatrist, who can keep an eye on it.
If you have any questions, please feel free to contact one of our offices located in Brighton and Greece of Rochester, NY . We offer the newest diagnostic and treatment technologies for all your foot care needs.